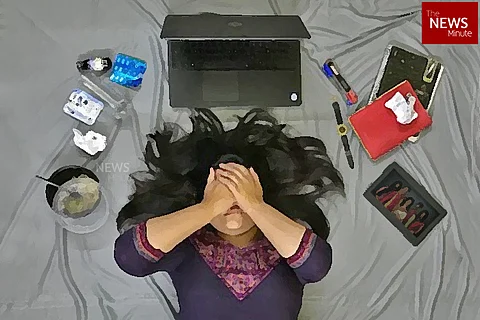
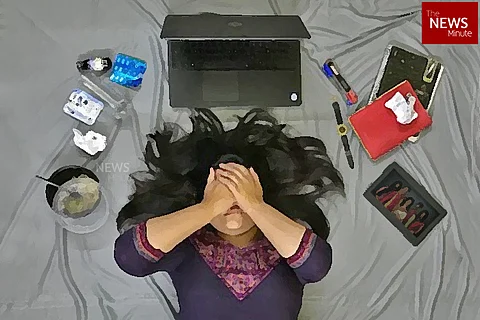
PMS, or Premenstrual Syndrome, has been the butt of enough sexist jokes. In common parlance, it has come to stand in for any time people believe a woman is expressing discomfort, irritation or “acting out”. The markers of PMS – cramps, mood swings, bloating, cravings, diarrhea – are many and varied. And Lalitha*, being a physician herself, knew this well. So, when she noticed marked changes in mood before her period in her early 30s, she tried taking steps to bring it under control.
“I cut caffeine, lessened my salt intake etc. but it didn’t make a difference,” she tells TNM. Living alone at that time, things got worse for the 38-year-old when she started feeling suicidal a couple of days before her period was due. “I was not able to get anything done; I wasn’t able to sleep, or I would sleep too much, and I did not feel like going to work,” she recounts.
This would happen for a week before her period, every month. “And after I got my period, it was like a cloud lifted from my head. The amount of work I could get done after that was phenomenal,” she observes.
This is one of the primary symptoms of PMDD, or Premenstrual Dysphoric Disorder. Defined by Johns Hopkins medicine as a “severe and chronic medical condition that needs attention and treatment”, its symptoms set in seven-14 days before menses, and subside once the person gets their period.
Thanks to Lalitha’s medical background and own research, she self-diagnosed herself with PMDD. “I felt validated that this is a real condition with a name… I was not going crazy,” she says.
However, there are many others whose PMDD is either diagnosed after a lot of trial and error, or not at all. Many a time, they may not even be aware of the link between their menstrual cycle and the deterioration of mental health preceding their period.
How PMDD is different from PMS
Bengaluru-based Dr Ashlesha Bagadia, a psychiatrist with specialisation in perinatal psychiatry and women’s mental health, explains that PMDD is different from PMS and is characterised by significantly more emotional distress and difficulty during the premenstrual time period. Crippling anxiety, increased irritability and/or overwhelmingly depressive or hopeless feelings are common symptoms.
“For example, something that may not be distressing otherwise starts distressing you a lot more during the premenstrual period in PMDD. There can be extreme shifts in mood… people may find it difficult to manage day-to-day things, which can disrupt work and also affect personal interactions,” she explains.
Up to two weeks prior to one’s menses, symptoms can present as intense fatigue, change in appetite, and so on. For some people, Bengaluru-based gynaecologist Dr Aruna Muralidhar says sleep cycles can be affected as well – people with PMDD may either sleep too much or significantly lesser than what is required on average. This makes PMDD quite interdisciplinary – it has strong aspects of, and repercussions on, mental as well as physical health.
The most telling characteristic about PMDD is what Lalitha perhaps described best: she felt like a cloud lifted from her head after she got her period. Both Dr Ashlesha and Dr Aruna agree that the symptoms dissipating as soon as one gets their period is a crucial factor in diagnosis. The experts caution however, that other hormonal and mental health disorders need to be ruled out before diagnosing one with PMDD.
PMDD does not affect a large number of women. Comprehensive figures are hard to come by due to lack of research. However, a UK research suggests it affects 1 in 20 women. Dr Aruna says that she has not seen more than six cases of PMDD in her 16 years of practice.
How PMDD affects people
PMDD can affect menstruating teens and people at any age, and can disrupt people’s lives significantly. For instance, Delhi-based Malvika* felt that everything she had worked on and towards for the rest of the month, would fall apart during the week before her period.
“I would go to sleep, feeling okay, and wake up the next morning to a feeling of doom – very immediate and very big – seven-eight days before my period. There would be no external trigger but I couldn’t help it. I’d end up sabotaging my relationships. My crying spells would increase, especially before going to sleep at night… they’d sometimes last for an hour and a half or more,” she narrates.
“Mentally, I felt like I was at zero. I could not concentrate on my work. Everything that I worked towards would get derailed in that week. I would have extreme anxiety and depression,” she says.
Malvika was diagnosed with PMDD three months ago by her therapist, about two years after her symptoms started showing. The 36-year-old had come across PMDD before while reading up on mental health. This prompted her to start maintaining a journal and noting down when she would have the peaks and dips in her mood.
“I noticed the pattern. When I told my psychiatrist six months ago, he said it could be related to my anxiety, contemplated that it could be borderline or bipolar disorder. But because I had been noting down the changes and when they happened in my journal, I told him that the symptoms manifested around my period,” Malvika says.
All this did cause strain in her personal relationships. Malvika tried to explain to her former partner that she was dealing with issues which get worse around a week before her period. “He didn’t understand, though he tried. We drifted apart,” she says.
Many people with PMDD are compelled to keep their illness secret, and the effort to maintain composure add to stress. “I have come across women who have not been diagnosed for a long time. Their quality of life has suffered. And as a result, they have marital discord and issues in personal and family relationships as well,” Dr Aruna observes.
While it took Malvika over a year to figure out what was happening, Bengaluru-based Sam suffered from PMDD symptoms for six years before he could get help. For the 32-year-old trans man, gender dysphoria (feeling of one's emotional and psychological gender identity being different to that assigned at birth) along with PMDD made it more difficult to seek medical help.
While Sam had painful PMS as a teen, things got worse in his twenties. “My symptoms used to start a week before menstruation date, and used to last for 21 days – one week before periods, one week during and one week after. I used to have migraines, fever, vomiting, fluctuation in blood pressure, body pain and mood swings. I used to feel so depressed and wanted to die sometimes. I used to be very violent,” he shares.
Sam’s PMDD had also caused a sleeping disorder, preventing him for sleeping more than three hours, compelling him to stay up for up to 48 hours, and be drowsy at work.
“Because of my gender dysphoria, I couldn't talk to my family. I was only talking about this to my psychiatrist and my partner. I was not able to go to work because of a fever. At work, I used to feel depressed, I used to feel like I wanted to die, and then all of a sudden, and I felt like I wanted to burn something,” Sam recounts.
The cyclical nature of PMDD also makes it tough to deal with – it is not like an illness which can be cured with a week-long medicine dosage; and even after the symptoms dissipate, you know that you will experience the same the following month. This takes a toll on intimacy and sex life too.
“Most people do not prefer having sex during menstruation, so that’s about a week gone. And when PMDD sets in for a week to ten days before the period… there is not much time left between couples with work and other routine. The other partner may not be able to understand this. It sets in motion a cycle of misunderstanding and puts strain on the relationship,” Dr Ashlesha says.
How PMDD is diagnosed, and is there a cure?
Considering the crippling nature of PMDD, the obvious question that arises is – is there a cure?
Experts say that there is no ‘cure’ as such, but there are ways of dealing with it. For some, like Lalitha, the diagnosis itself was a step in the right direction. However, she stopped experiencing PMDD after she had a child recently. Dr Ashlesha says that some people do get rid of PMDD at some point. “But we don’t know if it’s because of good treatment or some physiological changes,” she says.
But for most, since PMDD is a multidisciplinary disorder, the treatment follows suit.
Most women start with a gynaecologist because it’s a period-related problem. Dr Aruna starts by taking down their history which includes mental health, if they struggle with any addictions and so on. Apart from ruling out other issues like hyperthyroidism, Dr Aruna asks them to keep a diary for three-six months, to establish a clear link between their distress period and their menses. This is a practice Dr Ashlesha also follows.
In severe cases however, Dr Aruna says that they start the patient on birth control pills sooner, which help regulate the hormonal variation that could be causing heightened PMS or PMDD symptoms.
“We give those for two cycles and see if the symptoms resolve and then take a call whether to refer them to the psychologist or psychiatrist. After the diagnosis, we try and see if there is a possibility of them being amenable to continuing the contraceptive pills, which some of them might choose. Or we may start them on anti-depressants depending on our own competency in prescribing them. But, if they need additional therapy or counseling, then definitely it is multi-disciplinary treatment,” Dr Aruna explains. In some cases, a counselor gets involved from the very beginning.
Dr Ashlesha explains that while the established treatment are anti-depressants, it is better to take them for the entire menstrual cycle rather than just the time when PMDD symptoms appear, as the medication has a cumulative effect. “For many women, recognising that it’s linked to their period makes a lot of difference. Exercise helps too, as physiological symptoms like painful cramps get reduced and it has a positive effect on emotional wellbeing too,” she says.
This is what seems to be working for Malvika as well. A small dosage of SSRIs (Selective Serotonin Reuptake Inhibitors, a type of antidepressant), combined with the validation of the diagnosis and therapy, PMDD has become easier to deal with. “I know now this is going to come and go. And because we are working on the other things (through therapy), the dip is not as low as it used to be, and I am able to come out of it faster,” she shares.
Things were tougher for Sam, because he feared going to a gynaecologist or endocrinologist due to his gender dysphoria, even though his psychiatrist suggested it. Sam later went to an endocrinologist, and got a diagnosis. However, the treatment suggested to him was to take female hormones, which Sam obviously did not want.
Sam then started his Hormone Replacement Therapy (HRT), which stopped his period altogether. In the last 11 months, Sam says that he has seen a change in himself, where his anger issues are in control. He has also been regular to his BPO job, and is mentally in a better place.
Diagnosing PMDD correctly
Both Dr Aruna and Dr Ashlesha caution that one must ensure that PMDD is not a premenstrual exacerbation of an existing or underlying issue. This means that one could have an underlying health issue which could be more distressing in the premenstrual period due to the hormonal vulnerability during that time.
Incidentally, Malvika, Lalitha and Sam had struggled with some form of mental illness before their PMDD set in. While it is rare to find PMDD in its pure form, without any pre-existing psychological stressors, having a mental illness itself is not pre-requisite or a symptom of PMDD.
“For example, if you have hormonal imbalance or obesity, it can predispose you to PMDD. However, it is another thing to figure out with the obesity is causing the mental health problem or if obesity itself is a factor. In fact, in some cases, PMDD can be a sign of the onset of the bigger psychological disturbance,” Dr Ashlesha says.
The stigma they faced
Mental health and healthcare are often brushed off as a mood issue and thought to be the result of external triggers, rather than a legitimate problem. The stigma around going to therapy or taking medication for the same is also dominant. For Lalitha, this stigma prevented her from confiding in her near and dear ones too.
“I only told a colleague, no one else. Even though I am a medical professional, my family was very upset when I took on medication for depression in 2007. They were looking for a groom for me, and I definitely couldn’t tell this to a stranger,” she says.
While Lalitha’s colleague was supportive, she, too, discouraged Lalitha from taking anti-depressants. A few years since, Lalitha has now been married for four years. But even her husband does not know about her experience with PMDD. “We were in a long distance relationship for the initial part of our marriage, so it was easier to hide,” she says, “But if people were more accepting of this, I would have been more open about it.”
The stigma and shame often result in people being denied the right medical help as well. Like Sam, who preferred not to go a gynaecologist or an endocrinologist, Malvika was also wary when her psychiatrist suggested she consult a gynaecologist. “The gynaecologist knew people in my family and social circle,” she offers as an explanation.
Fortunately for Malvika, at some point she decided to tell the people close to her what was happening. “It’s been liberating to get this off my chest than taking care of what others are thinking,” she says. “You just need to take charge sometimes. Ultimately, it’s about self-care. And now that I know about this, I am trying to encourage a niece who is going through mental health issues herself, to seek help.”
Dismissal of women’s pain, lack of awareness
It does not help that sometimes medical professionals themselves are dismissive. There is plenty of anecdotal and academic evidence to suggest that the medical fraternity often dismisses women symptoms and pain, for a variety of reasons including branding them as ‘too dramatic’.
For instance, when Malvika went to a psychiatrist for an eating disorder seven-eight years ago, she got a lecture on eating right. And when Lalitha tried to get help for her excruciatingly painful menstrual cramps, she was told everyone has cramps, and she should just put up with them. “In my early 30s, things were so bad that I was fainting from cramps. A lot of people, including some gynaecologists told me that I just needed to get married and things would be fine,” she says incredulously.
Not only is awareness about PMDD lacking when it comes to the general public, but Dr Ashlesha and Dr Aruna agree that it is not up to the mark in the medical fraternity either.
For starters, Dr Aruna points out, mental health usually does not even form part of the medical history taking. “Personal history taking should include stress levels, incidence of domestic violence, history of addiction etc. Though it’s tough to do in a busy practice, we need to take time to build a rapport because these things may not come out immediately. Even women do not tell us these issues initially unless we delve into it,” she notes.
Lalitha points out that women’s health does not get as much attention in research because most research is driven by pharmaceutical companies. “Any medication that can be taken long term is profitable – so you see lots of research in say, cardiology. Something like endometriosis and PMDD do not affect all women. And because of the stigma around it, medication is not as popular,” she explains. “Also, more often than not, the decision makers in companies tend to be men. So, they may not think of these issues as particularly important,” she adds.
The debate around PMDD being a mental health issue
PMDD was classified as a mental disorder in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM - 5) by the American Psychiatric Association (APA) in 2013. It had been introduced as a “depressive disorder not otherwise specified” in the manual’s fourth edition (DSM-4). PMDD had also been introduced for the first time into the International Classification of Disease (ICD-10) by the World Health Organization (WHO). According to an Indian study published in the Indian Journal of Psychiatry, the prevalence of PMDD in women in India was found to be 3.7%, based on the directions given in DSM-4 and ICD-11.
Interestingly, after the APA classified it as a mental disorder in 2013, the International Classification of Disease (ICD-11) by the World Health Organization (WHO) also included PMDD in its draft published in 2017, that will be presented to member nations in May 2019. “The symptoms are severe enough to cause significant distress or significant impairment in personal, family, social, educational, occupational or other important areas of functioning and do not represent the exacerbation of a mental disorder,” the ICD says.
Earlier this year, in a paper authored by two persons from the Department of Psychiatry at NIMHANS, the authors say: “This is one condition which definitely needs more research to ensure that medicalisation of menstruation and the menstrual cycle does not happen and women are not unnecessarily labeled with a diagnosis of a mental disorder.”
While there have been debates earlier that not all of women’s pain could be construed as something “mental”, the ICD-11 and DSM-5 classification could pave way for more research.
*Names changed